Monthly Updates January 2026
Welcome to the January 2026 edition of the EAED Monthly Bulletin. This newsletter includes update from the Executive Committee (EXCO) and all other Working Committees, information about our next spring meeting in Barcelona, Pearls from our official jourmal IJED and important news from our GOLD and SILVER partners.
Committees Updates
The EAED has several committees: Executive committee, Financial Advisors, Membership Committee, Affiliate Committee, Media Committee, Candidate Committee, Innovation Committee & Sponsorship Committee,
Executive Committee
Dear members, affiliates and partners,
As we end the holiday season, I wish to reflect on what has been achieved during the past year and consider what lies ahead when entering 2026.
With regard to the numerous projects undertaken by the Exco and committees to renovate the structure, visibility and administration of our academy, significant progress has already been made, and we are working tirelessly to successfully complete this transition and improvement process. We would like then to thank you for supporting the update of our new membership platform and for your positive feedback about our new website. If these services occasionally underperformed, we thank you for your patience while our partners and Exco members worked in real time on the necessary corrections.
During the second half of 2025, you received our newsletters, which became a key communication tool for connecting our community and partners and providing them with meaningful information about the life and activities of the EAED. They also enabled members and affiliates to stay connected with our industry partners and learn about new products and developments of interest to aesthetic dentistry. Thank you, Rafi Romano and team, for concretizing this important project successfully.
Another crucial improvement to our administration was the hiring of Renate Androsch-Holzer, our new secretary, whom you met for the first time in Split and then in Algarve. She has quickly become an integral part of our academy, providing efficient and attentive support…always with a smile! In 2026, we look forward to further developing and improving our services to facilitate all administrative processes for EAED fellows.
For our next meetings in Barcelona and Crete, the organizing committees worked hard to prepare outstanding scientific and social programs, as well as selecting very special venues, maintaining EAED's tradition of high quality events. Please visit our website at your earliest convenience and register early, as places are expected to fill up quickly (https://www.eaed.org/meetings/annual-meetings).
Before closing this note, let me thank again my Exco partners, advisors and all committees’ members, as well as our secretary, for their year-round dedication and hard work in making this Academy a unique group, proudly dedicated to improving aesthetic dentistry.
I wish you all I wish you all a beautiful start into 2026! May the New Year bring us all health, peace, and success.
Didier Dietschi, President

Innovation Committee
We are pleased to announce the formation of a new Innovation Committee (IC), dedicated to identifying, evaluating, and promoting innovations developed by our members and affiliates. The IC will serve as a platform to highlight pioneering concepts, techniques, and technologies within our community. Members and affiliates who wish to present their innovations at upcoming meetings are invited to submit their proposals for review by the committee. In recognition of this new focus, the John McLean Honorary Lecture will henceforth be known as the John Walford McLean Innovation Honorary Lecture, honoring both tradition and progress through innovation. The IC is now open to receive submissions for consideration for the Geneva meeting. The selected innovation lecture for the Barcelona meeting will be presented by Dr. Galip Gurel.
Members are warmly invited to submit their proposals to any of the IC members:
Prof. Nitzan Bichacho nitzan@bichacho.clinic
Prof. Irena Sailer irena.sailer@unige.ch
Dr. David Winkler drdavesmile@gmail.com
MDT. Vincent Fehmer vincent.fehmer@unige.ch
Prof. Lorenzo Breschi lorenzo.breschi@unibo.it

Membership Committee
How to become an Active member of the EAED?
After your sponsors have submitted your application, and if it is approved by the Membership Committee, you will be invited to deliver a brief, professionally oriented presentation on a topic related to esthetic dentistry that reflects your clinical or scientific work. If the candidacy is approved, the candidate will be given notification of the date and place in which he/she will present in front of the MC. Slots are limited and are filled on a first come first serve basis. The sponsors and the EAED Membership Committee will provide guidance on the style and duration of your intervention, which should follow the guidelines outlined here...
In Barcelona Spring meeting, 8 affiliates members will be screened by the committee for active member candidacy.

Affiliate Committee
The Affiliate Committee meets approximately once a month by Zoom to discuss current state of affairs, initiatives, etc.
At the moment there are 13 colleagues who have expressed an interest in attaining Affiliate status, have attended at least 2 Spring Open Meetings, and have submitted 3 sponsors signatures to support their application. These will be posted online so that Active and Life Members can vote on the applications during the 2026 Barcelona meeting.
We would like to remind all Affiliates that we would love to arrange a 1-2-1 Zoom with you to discuss your cases, your collaboration with your sponsors, and how to progress on your journey towards Active membership. Please email us at affiliates@eaed.org to arrange a date and time that suits you.
Dave Winkler, Life Member UK
Sponsorship Committee
The Sponsorship committee together with the EXCO are completing the list of partners and exhibitors for the Spring meeting in Barcelona. Among them you can find:
6 Gold Partner: Align Technology, Meisinger, Thommen Medical AG, SprintRay, Nobel Biocare, Straumann
1 joint Gold Experience Booth: Zeiss, Ivoclar, HuFriedyGroup
5 Silver Partner: OsteoBiol by Tecnoss, Deppeler, Aidite, Dexis, Coltene
7 Exhibitors: American Dental Systems GmbH, Dr. Jean Bausch, Micerium S.p.A., Ultradent Products GmbH, Solventum Germany GmbH, Ustomed Instrumente, Brumaba GmbH & Co. KG
1 Media Partner: Quintessence
In the next newsletter we will share the details of every one of our partners and exhibitors so that all attendees will be able to visit them and learn about their innovaitons and products.

ANGLE-net Session!
The EAED participated in the ANGLE-net Session moderated by our life members, Prof. Nitzan Bichacho and Dr. Renato Cocconi. The next session is on February 2nd. The topic is "Gingival Tissue Management in Orthodontic Patients: An Interdisciplinary Approach"
Speakers: Christos Katsaros & Anton Sculean
Moderator: Stella Chaushu
Regotsration is free at the link...

Honorary Member- Dr. Robert Gottlander
My journey with EAED started in 1998 in Paris at Hotel Lutetia. At that time I was working with esthetic implant solutions and was recommended to take part in this meeting. The quality of the presentations and the quality of the members made an incredible impression on me.
This was a milestone in the work we did at Nobel to move to esthetic and prosthetic focus in implant treatment. Several members of EAED also got more involved in esthetics on implants. This changed the view on implant treatment from surgical to a more prosthetic approach, which still remains today. Over the years it has been a very fruitful cooperation between EAED, its members and the industry, something I truly believe has made a difference for the most important group -the patient.
For me personally I recognized already in Paris that EAED was different from many other dental organizations. There was a very open atmosphere where it was possible to discuss clinical success but also challenges as well as how to overcome these challenges, all done with respect and with the purpose to get to a solution.
The other unique part is the accessibility to people with very high knowledge, at the meetings is it very easy to ask and discuss topics - and to learn a lot. I have recommended many colleagues to participate/ join because there are very few places you can learn as much about today’s dentistry as you can at an EAED meeting
At last but not least is this a place where you have unique social events but even more important a place where you develop lifelong friendships - EAED Family is not only a phrase, it is for real.
I am honored to be an honorary member. I thank EAED for giving me the is honor and I look forward to continue the journey together for many more years


Barcelona Spring meeting 28-30 May 2026
The organizing committee, Dr. Didier Dietschi EAED President, Dr. Andrea Ricci, President Elect and Co-scientific Chair , Dr. Cristina Lopez Local Chair, & Dr. Nikolaos Perakis Co-scientific Chair, are happy to invite our active and affiliates members and guests to secure their place for this outstanding meeting which will be held from 28-30 May 2026. .
As the new year begins, preparations for the next EAED Spring Meeting 2026, are already in full swing! The conference theme, “Esthetic excellence made predictable”, promises a program full of expert talks, cutting-edge discussions, clinically relevant insights and new techniques. Explore the Scientific Program with an overview of the key topics and high-class speakers.
Secure one of the last hotel rooms at the Majestic Hotel & Spa!
Accommodation at the official headquarter hotel, the Majestic Hotel & Spa, is nearly at capacity. If you wish to stay at this hotel, register as soon as possible or reach out to us by email.
Take Part in the EAED Photo Contest: We invite you to submit your most impressive clinical photographs to the EAED Photo Contest 2026 by sending your submissions by email. Whether it’s an outstanding result, an elegant case, or an artistic piece — let your images speak for your expertise. We look forward to sharing further updates as the meeting in Barcelona approaches.
For more information and registration click here...
Algarve closed meeting Scientific "Pearls"
(part II)
1. Dr. Inaki Gamborena (SP)
Immediate Implant Placement in Hopeless Teeth: A Risk-Based Decision Algorithm
This lecture delivered a clear, practical framework to decide whether a compromised tooth qualifies for safe immediate implant placement or requires strategic staged reconstruction to prevent tissue collapse prior to implant placement or a conventional 3 unit bridge.
Focusing on critical diagnostic thresholds (buccal plate, biotype, socket type, apical pathology, bone-marginal soft tissue relationship), you’ll master a repeatable risk-stratification tool that predicts esthetic and functional outcomes with confidence.
Walk away knowing exactly when “immediate” is truly low-risk — and when staged regeneration is mandatory to preserve hard and soft tissue integrity.
2. Dr. Raphael Wymann (CH)
Diagnosis & treatment options to improve a cracked tooth ’lifespan‘
Cracked teeth represent a very challenging condition in restorative dentistry, as untreated cracks may compromise pulpal vitality and can ultimately lead to tooth loss. This lecture presents an evidence-based treatment protocol and a novel, clinically oriented classification system specifically designed for vital teeth with structural cracks.
Beginning with the aetiopathogenesis, contemporary diagnostic strategies are critically examined. Building on this foundation a structured decision-making is presented, integrating material selection and the appropriate level of therapeutic invasiveness required to achieve biologically sound and predictably stable outcomes.
A series of clinical cases illustrates the practical implementation of the proposed classification and highlights its value in enhancing prognostic accuracy and optimizing clinical management.

3. Dr. Jorge André Cardoso (PT)
The non-vital tooth and options to increase its lifespan
Root canal treated teeth present specific biomechanical and optical challenges. During the lecture several aspects were discussed for both posterior and anterior teeth:
- Factors increasing risk of fracture
- Remaining tooth structure and restorative options
- Cusp coverage and "ferrule" designs
- Adhesive versus retentive restorations
- Controversy on the use of posts and/or fiber-reinforced composites
- Preparation designs according to each clinical scenario
- Specific challenges in anterior and posterior teeth
- Most recent evidence from in vitro and in vivo studies

Algarve New Active members' presentations
1. Dr. Lara Stangacilovic (RO)
Choosing the Right Treatment Plan to Meet the Patient’s Expectations
effective communication among the interdisciplinary team involved in a complex rehabilitation case is often the key to success. This case builds on this idea and shares our philosophy and workflow as a true interdisciplinary team in which we all aim to deliver the best treatment option that successfully meets the patient’s expectations.
As doctors, we all take pride in our ability to design an appropriate treatment plan for our patients, but we often face the challenge of aligning this with the patient’s expectations and identifying the right course of action to deliver on that. In order to arrive at a proper diagnosis and make appropriate clinical decisions, we need to look beyond the smile and consider the entire face of the patient. When talking about facially driven full-mouth rehabilitation, we must pay special attention to establishing the nature of the concern—whether it is purely dental, skeletal, or both—to select the appropriate treatment and achieve the best functional and esthetic results for our patients. Where skeletal issues are concerned, simply trying to improve one aspect will almost certainly result in failure.
for more details of the above case: Quintessence of Dental Technology 2024 | Volume 46

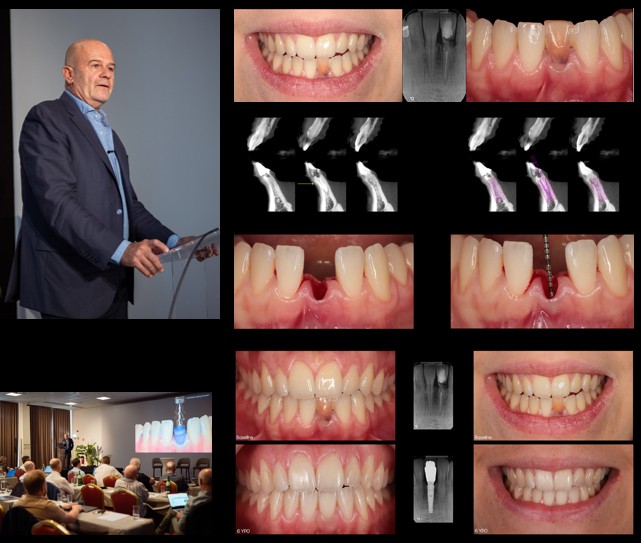
2. Dr. Jean-Pierre Gardella (FR)
Replacement of an hopeless lower incisor for structurally reasons
This case is related to the replacement of an hopeless lower incisor for structurally reasons, with of course, a reduced surgical and prosthetic space, which is one of the most challenging clinical situations when we have to replace a single tooth. In addition, the phenotype in this area is definitively thin as usual and every surgical approach concern should be not only conservative but should have an overcorrection purpose both for hard and soft tissues.
treatment plan:
1. periodontal phase, to reduce the plaque-induced inflammation, with the splinting of tooth 31 following coronoplasty, to eliminate the contacts in MI and so to decrease the pain: this phase was performed on the day of her first visit.
2. Extraction of tooth 31,immediate implant placement, and temporization of this implant as well, if the surgical context is favorable, I mean: preservation of the buccal plate after extraction, and a good primary stability.
3. Final implant restoration.
4. A periodontal and implant supportive treatment.
The CBCT cuts show the thinness of the buccal plate and the surgical planning using a 3 mm implant diameter as the best tool for both surgical and prosthetic aspects. After an atraumatic «flapless » extraction, the integrity and level of the buccal wall is checked, using a periodontal probe: this point is crucial for the ideal 3D implant positioning. The small diameter implants placed with a good primary stability; a soft tissue graft is harvested form the tuberosity and placed on the buccal aspect: note that a small part of the CTG remains exposed in order to increase the quantity of KT.
A conventional impression is taken immediately after the surgery, and a few hours later, the provisional is screwed in. At 6 days post-op the healing shows a perfect integration even at the exposed soft tissue graft area. At 4-month post-op the soft tissue maturing is very nice, and an analogic impression is used for the final restoration.
The quantity of keratinized tissue at 6 years follow up has been augmented due to the exposed part of the connective tissue graft. The patient can smile again without any limitation.
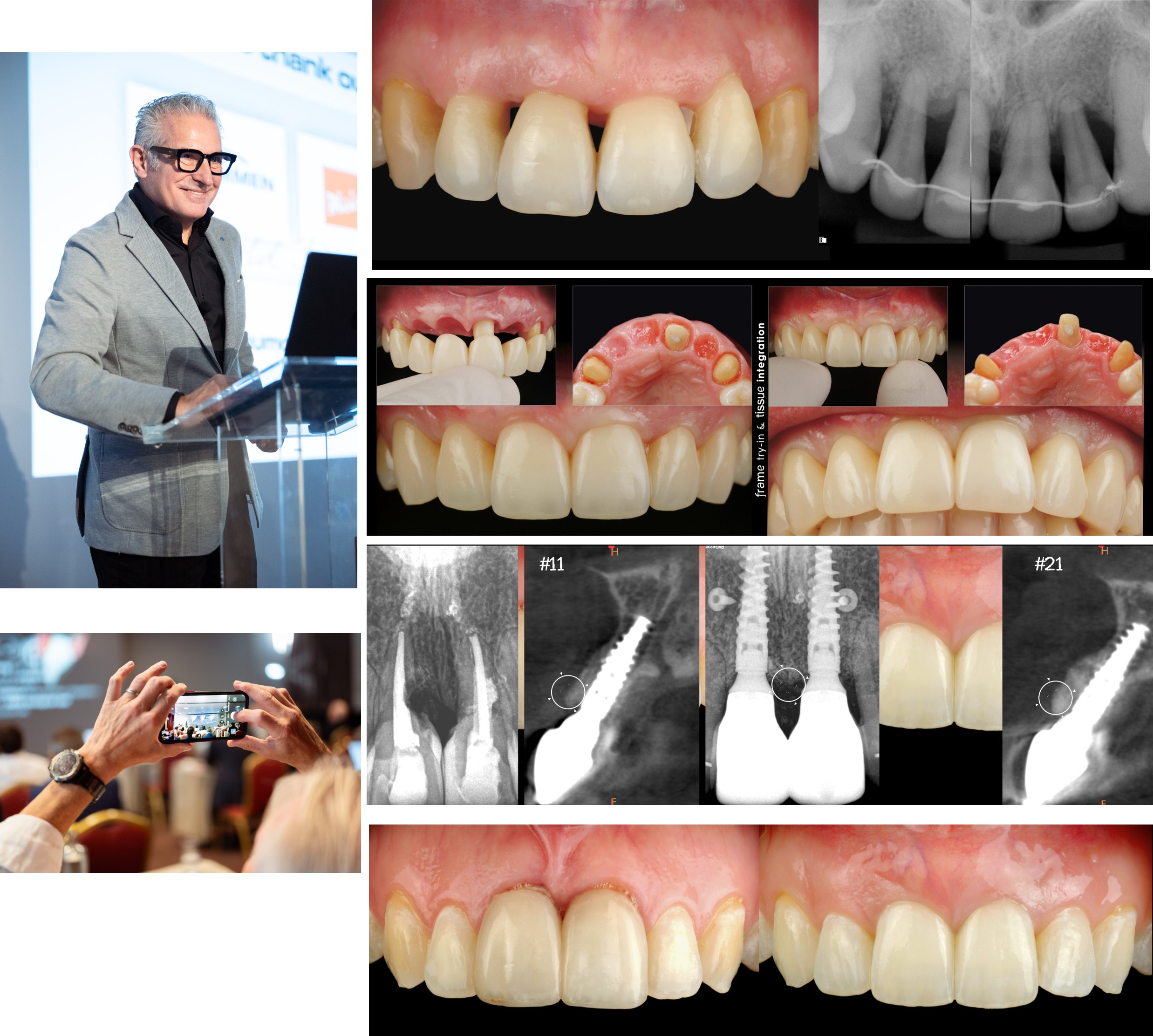
3. Dr. Gaetano Paolone (IT)
Interdisciplinary Management of a Complex Aesthetic and Restorative Dilemma
The patient presented to the clinic after losing a veneer (#1.1) during a surfing activity, reporting both aesthetic discomfort and concerns about the integrity of the affected tooth. Clinical evaluation also revealed additional restorative needs involving several posterior and mandibular anterior teeth.
An indirect adhesive restoration was selected for the maxillary central incisor, where a feldspathic CAD/CAM veneer was fabricated to accurately reproduce tooth morphology, optical characteristics, and enamel-like translucency. The restoration was bonded using a full adhesive protocol to ensure optimal retention and seamless integration with the adjacent teeth. Mesial portion of #2.2 was also restored directly.
In the posterior region, direct adhesive restorations were performed on multiple teeth presenting with interproximal Class II lesions and compromised contact points. Composite resin was used to rebuild the proximal walls, re-establish anatomical contact relationships, and restore proper occlusal function.
Direct composite restorations were also carried out on the mandibular incisors to manage wear and minor structural defects. Modern layering techniques allowed precise control over shade, translucency, and texture, ensuring a natural integration with the existing dentition.
The combination of indirect feldspathic veneer rehabilitation and direct adhesive restorations on posterior and anterior teeth enabled a minimally invasive, functional, and highly aesthetic outcome, fully restoring the patient’s smile after the traumatic loss of the original veneer.

4. Dr. Maxim Kopylov (RU)
Patient: Male, 48 years old.
Chief complaints: Unsatisfactory esthetics, impaired mastication, gingival bleeding, and teeth mobility. The patient expressed fear of losing all teeth. Treatment expectations: Highly motivated and willing to undergo prolonged treatment to preserve the maximum number of natural teeth. Previous consultations: The patient had been advised at other clinics to extract all remaining teeth, place 4–8 implants per jaw and perform full-arch implant-supported prosthetic rehabilitation.
Treatment plan:
1. Reinforcement of the patient’s motivation for oral hygiene
2. Substantial improvement of home-care skills (professional dental prophylaxis
and oral hygiene instruction)
3. Extraction of hopeless teeth
4. Provisional prosthetic rehabilitation
5. Alveolar ridge reconstruction (bone augmentation of alveolar defects)
6. Orthodontic treatment in the mandible
7. Implant placement in adequate prosthetically driven positions
8. Transitional restorations
9. Definitive restorations: veneers on natural teeth and implant-supported crowns
The presented interdisciplinary strategy enabled maximum preservation of the patient’s remaining dentition in both arches while creating the biological and prosthetic prerequisites for a predictable implant-supported rehabilitation. Extensive alveolar defects were successfully reconstructed, providing sufficient hard-tissue volume for prosthetically driven implant placement. In addition, the proposed combined vestibuloplasty technique achieved an adequate zone and thickness of peri-implant keratinized/attached soft tissues, which is considered beneficial for long-term soft-tissue stability, hygiene access, and maintenance of peri-implant health. Importantly, these objectives were accomplished within a condensed clinical timeline, avoiding unnecessary prolongation of an already complex rehabilitation. Finally, the treatment process resulted in a profound improvement in the patient’s health behavior, with sustained motivation and adherence to oral hygiene measures for both teeth and implants, supporting long-term functional and esthetic outcomes

EAED active members case presentations
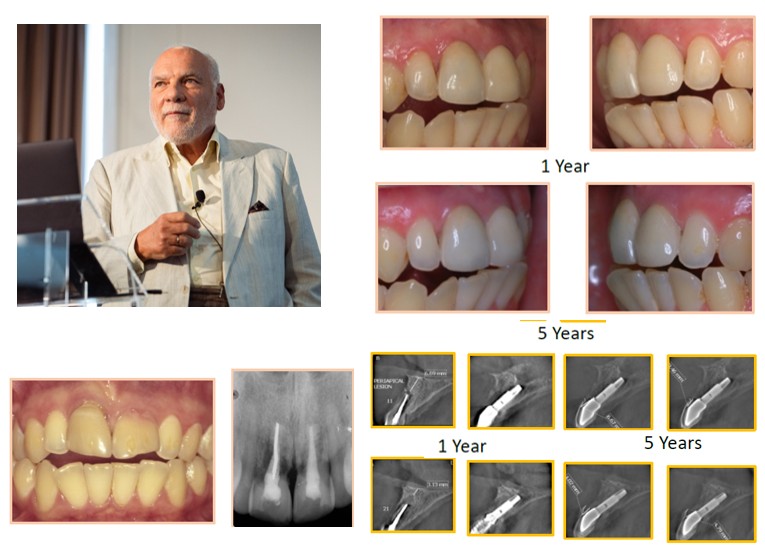
1. Prof. Aris Petros Tripodakis (GR)
The structurally compromised tooth: Extraction & implant strategies for "irrational to treat" teeth”.
Principles of the guided healing and management of the soft tissues by prosthetic means can be successfully applied in the direct transformation of periodontal tissues into peri-implant tissues by the immediate intra-socket implant restoration in structually of compromised sites. (Tripodakis APD, Immediate implant placement combined with controlled immediate loading in infected and defective sockets. Part I: Single tooth (N=13), Implantologie 2001; 1:13-25 & Part II: Multiple adjacent teeth (N=20), Implantologie 2002; 3:271-286).
Microbiological findings have shown that the previously housed periopathogenic flora associated with the site pathology of the extracted periodontally involved tooth, did not hinder the process of osseointegration. One year post-operatively the intracrvicular flora was found to be less pathogenic, compatible with the attained health of the periimplant tissues. (Tripodakis AP, Nakou M, Microbiologic evaluation of compromised periodontal sites before and after immediate intrasocket implant placement (N=20) Int. J. Perio Rest Dent 2011;31: e109– e117)
The retrospective evaluation of the distance of the labial hard and soft tissue margins from the implant shoulder in maxillary anterior periodontally compromised sites that were restored by immediate flapless implant restorations, combined with inorganic filler labially, was evaluated in a case series study (N:20) by volumetric analysis 5 years postoperatively, using cone beam computed tomography. Volumetric findings, five years postoperatively have confirmed the presence of the buccal bone (preserved or newly formed) coronally to the implant-transmucosal abutment junction supporting a stable soft tissue free periimplant crest in combination of shallow crevice. In all cases, a labial radiopaque plate component was apparent 5 years postoperatively coronal to the implant shoulder 3.1 ± 0.6 mm, supporting the soft tissue margin, which was extending above this level 5.2 ± 1.1 mm (Tripodakis et al. Five-year volumetric evaluation of periodontally compromised sites, restored by immediate implant restorations (N=24) Int. J. Perio Rest Dent 2016; 36:644-653)
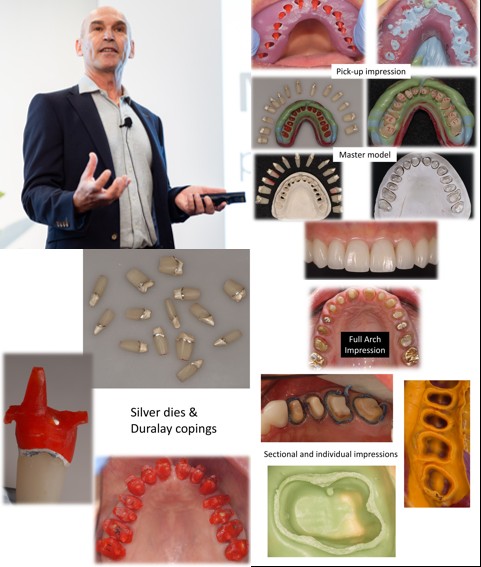
2. Dr. Basil Mizrahi (UK)
Full Arch Impressions of Biomechanically Compromised Teeth
Full arch impressions are stressful, unpredictable and fraught with difficulty. Although Digital scanning is replacing traditional silicone impressions, there are situations where it cannot match the precision of a silicone impression. Ie:
• Deep subingival due to decay or pre-existing crowns
• On posterior teeth where PFM crowns with precise metal castings are fabricated to fit mechanically resistant preparations with retentive grooves.
This is a refinement/update of an old technique popular in the 1960’s. Refinements have been designed by Mr Salvatore Sgro (Technician, Rome, Italy) and Dr Basil Mizrahi and include :
• use of a specially designed custom tray that allows the resin pick-up copings to be luted to the impression tray for extra rigidity
• Linking of sections of the copings to prevent dislodgement during light body application.
• A verification jig to insure precision of pick-up impression
The technique involved taking multiple individual or small sectional impressions. These impressions are then silver plated for strength and durability. Individual, silver plated, dies are then made from the multiple impressions. On each die an extremely accurate Duralay pick-up coping is made. These copings are then reseated intraorally over the teeth and a pick-up impression is made. The main advantage of this technique include is the avoidance of having to capture multiple teeth in a single impression.
Following the presentation a lively debate ensued around the merits of analogue vs digital impressions. Basil defended his presentation saying that severely failing dentitions are beyond “ minimal invasive dentistry “ and often unsuitable for adhesive dentistry. For these cases he prefers a traditional mechanical crown and bridge approach and for this analogue impressions are superior for the reasons outlined above.
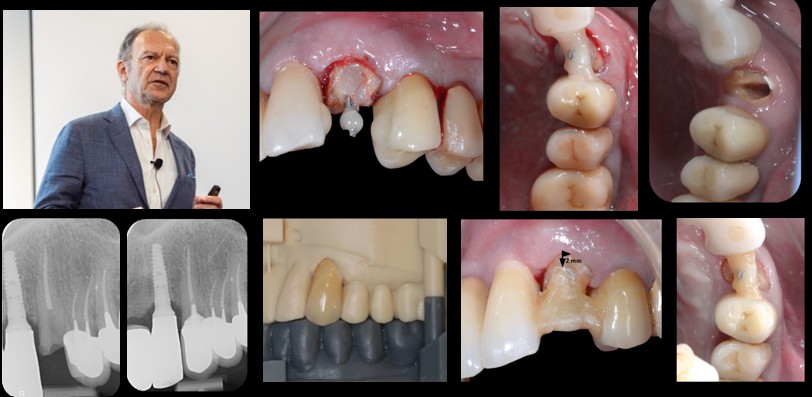
3. Dr Tidu Mankoo (UK)
Interdisciplinary Management of a Complex Aesthetic and Restorative Dilemma
Diagnosis: Patient’s concerns, history and background: First seen in 2010. 48 year old female, lives in N Ireland (so has to fly to LHR to see us), referred by colleague who treated her there. NRMH, ASA 1, fit and healthy. History of failed restorations including bridge 13-11 and at presentation 12, 11, 24, 25, 26 have been lost. 2 failed grafts in 12-11 area, initially by referring GDP and then by implant specialist. No financial limitations. Wants single teeth, prefers not have bridgework.
Prognosis: Periodontally: good; Dental: good (for teeth present and existing implants) with the exception of 13 which is guarded due to post. proximity to root wall. Surgical prognosis: very guarded for 12-11 with high risk of morbidity & complications; good prognosis for 24-26 ; Aesthetics: good
Treatment options:
-Comprehensive restoration of upper arch & lower posterior teeth with crowns, new fillings etc.
- Additional implant at 24 along with horizontal hard/soft tissue augmentation
Main issues relate to anterior defect management
‣ Repeat surgery 21-11?
‣Prosthetic gingivae with new bridge 13-21
‣ Do we keep the tooth 13?
‣ What else can we do?
‣ Can orthodontics help us?
‣ Move 13 into position of 12?

4. Dr. Grégoire Audi (FR)
Surgical Extrusion of a Compromised Anterior Tooth
This case report describes the management of a compromised anterior tooth (tooth #23) previously restored with a post-retained crown, which presented with a subgingival fracture. Crown lengthening was initially considered; however, it was contraindicated due to an unfavorable crown-to-root ratio. As an alternative, surgical extrusion was performed to reposition the remaining root structure coronally.
The tooth was stabilized by splinting it to adjacent teeth, allowing for periodontal healing. A definitive crown will be placed upon completion of the healing phase. This approach preserved the tooth and restored function and esthetics without the need for extraction.
EAED Partners
Our partners fuel the Academy’s growth
and evolution.
Thank you for making it possible.


Master Class on Tour with Dr. Istvan Urban and Prof. Dr. Fouad Khoury
The GBMN Master Class on Tour 2026 brings together two leading experts in regenerative dentistry – Prof. Dr. Fouad Khoury and Dr. Istvan Urban – for an exclusive educational tour through Paris, Milan, Düsseldorf, and Warsaw.
Look forward to:
• Two intensive days of lectures by Prof. Khoury and Dr. Urban
• Hands-on training: Choose one hands-on workshop with either Prof. Dr. Khoury or Dr. Urban
What is the GBMN? The Global Bone Management & Restorative Network is an open, independent academy for evidence-based dental education, connecting professionals worldwide to advance the quality of dental care. Join this unique opportunity to learn directly from two of the field’s most influential practitioners. All dates and locations:
Paris: May 29th – 30th
Milan: June 12th – 13th
Düsseldorf: September 4th – 5th
Warsaw: November 6th – 7th
Visit the GBMN website for more information and registration...

INICELL® Surface
The INICELL® Surface from Thommen Medical supports a rapid healing process. It is generated with an alkaline solution in the chairside APLIQUIQ® system. Compared to the unconditioned surface, INICELL® is a super hydrophilic surface that strengthens homogenous protein absorption. It also increases the blood clot on the surface for faster osseointegration. Do you want to know more?

Transforming Restorations with iTero Lumina™
Discover how innovation meets efficiency in this clinical case by Dr. Yi Jyun Chen. Leveraging the Align Digital Workflow, the team delivered same-day, 3D-printed resin crowns—a breakthrough in pediatric care.
With the iTero Lumina™ intraoral scanner, clinicians gain:
- 3X larger field of view for faster, more comprehensive scans
- Photorealistic images that elevate patient confidence
- Unmatched full-jaw accuracy for predictable, first-time fit
Combined with Align Oral Health Suite and iTero Design Suite, this workflow reduces chair time, enhances communication with parents, and ensures aesthetic, well-fitting restorations—all in a single visit.
Why it matters:
• Comfortable scanning experience thanks to ergonomic design
• AI-driven processing for speed and precision
• Integrated tools like Invisalign® Outcome Simulator Pro for next-level treatment planning Ready to redefine your restorative workflow?[click below to learn more about iTero Lumina™ )


A New Standard in Chairside Aesthetics: Crown HT – The first Midas-Exclusive Resin Now EU MDR Class IIa Certified
SprintRay’s new high-translucency restorative resin Crown HT — developed exclusively for the Midas Digital Press system—has officially received EU MDR Class IIa certification.
This marks an important step for aesthetic-focused clinicians who want to deliver beautiful, lifelike restorations in a single visit.

You already have the power
Straumann helps you to unleash it. Straumann iEXCEL™ unlocks unique next-level efficiency, control and confidence. Turning your talents into superpowers, and your vision into reality that changes lives for the better.

With Nobel Biocare you can confidently deliver a beautiful smile to your patient on the day of their surgery, using our esthetic digital workflow
Gold Experience Booth
Ivoclar complete product systems work together in concert to ensure efficient and reliable results. Our smart systems are designed for entire workflows. All steps from initial consultations with the patient to after-care are covered simple and intuitive processes save you time and deliver reliable results
Perfectly matched products create additional value.

Over 70% of dentists suffer from musculoskeletal disorders due to awkward positioning and poor posture. ZEISS UP with the dental microscopes from ZEISS and reduce back and neck pain. By sitting upright and maintaining a neutral posture, you can fully focus on your patient and the procedure

HuFriedyGroup is proud to introduce the EFP Probe, a cutting-edge periodontal instrument developed in partnership with the European Federation of Periodontology (EFP), a global non-profit organization with a European core that promotes periodontal science and practice, and awareness of oral health and gum disease. Aligned with the current periodontal classification and the EFP’s clinical practice guideline, the EFP Probe is designed to help clinicians seamlessly translate state-of-the-art periodontal diagnosis and treatment decision-making into everyday clinical practice. It is suitable for use in all phases of periodontal and peri-implant therapy.
The EFP Probe features:·
A marking at 3 mm·
A black band from 4–6 mm, with a distinct marker at 5mm·
Millimeter markings from 7–15 mm, with black bands at9–10 mm and 14–15 mm
Learn more about EFP Probe...

Deppeler products are made in Switzerland since 1934. We develop our instruments in partnership with dentists and universities. Our steel is perfectly balanced between flexibility, durability and tactility.
for more information on our new spatula click here...
For a video explaining the use and design of the spatula by Dr.Martin von Sontagh click here...

OsteoBiol® by Tecnoss® provides Dual-Phase collagen-based biomaterials, the result of extensive research that has enabled the preservation of natural collagen within the bone matrix.
OsteoBiol® products are made of animal origin and are available in a wide range of packagings and sizes, because different clinical applications require different regenerative solutions.

Aidite (Qinhuangdao) Technology Co., Ltd., founded on March 15, 2007, is a leading global provider of integrated dental solutions, specializing in the R&D, manufacturing, and servicing of dental materials and equipment.
Aidite holds 153 valid patents, reflecting its strong commitment to innovation in the dental industry. Its products are exported worldwide, supported by four overseas subsidiaries in the United States, Germany, South Korea, and Japan, and technical service teams across India, the Middle East, Australia, South America, Vietnam, Brazil, the Arab region, and Thailand.
Aidite continues to advance product innovation, technology, and business models. Through ongoing R&D investment, the company works toward its vision of fully applying digital and intelligent technologies in oral healthcare, empowering technicians and dentists with high-quality, convenient, and personalized solutions.


DEXIS Imprevo Intraoral scanner
Dental professionals around the world rely on Imprevo for efficient, accurate intraoral scans. Powered by parallel processing and dual sensor technology, this DEXIS´s latest intraoral scanner is built to empower your workflows with clarity, confidence, and a clear path to ‘yes’.
Learn more about DEXIS Imprevo
Kerr introduces OptiBond™ Universal 360, a revolutionary bonding solution designed to meet the highest demands of modern dentistry. Built on the trusted OptiBond technology and now enriched with MDP, this universal adhesive ensures exceptional bond strength across all etching techniques, materials, and applications.
Learn more about OptiBond™ Universal 360


COLTENE is an internationally active company specialising in the development, manufacture and distribution of dental consumables and small devices in the areas of Dental Preservation & Improvement, Treatment Auxiliaries, and Infection Control. COLTENE operates state-of-the-art production facilities in the US, Canada, Germany, France, Hungary, and Switzerland and is present in the important key markets in Europe, North America, Japan, China, and India with its own sales companies. Dental practices, DSOs, dental clinics as well as dental laboratories rely on high-quality products from COLTENE.


Quintessence Publishing is a family of authors and professionals who work together to bring you the latest and greatest information in dentistry.
Here are some of our new titles:
1. Vincent Fehmer
Optimizing Clinical and Laboratory Workflows
2. Arun K. Garg
Full-Arch Implant Rehabilitation
3. Charles J. Goodacre / W. Patrick Naylor
Single-Implant Complications
Social Media
The goal of this section is to bring our readers eye-catching and high quality images related to novel techniques, clinical challenges and emerging trends relevant to esthetic dentistry. You would like to submit an outstanding dental photo? Please contact IJED Editorial Manager: ladetzki@quintessenz.de
The International Journal of Esthetic Dentistry | Volume 19 | Number 1 | Spring 2024|
Photographer: Joshua Polansky
Camera: Nikon D800
Lens: Nikon 15 VR
Flash: Backlit with Nikon R1C1 Flash
Aperture: 22
ISO: 300

The resolution of endo-periodontal lesions“
by Rodrigo González Terrats, Beatriz Martínez, Beatriz De Tapia and José Nart recently published in IJED 04/25
Editorial Manager Dr Kristin Ladetzki had the opportunity to talk to José Nart at SEPES Bilbao: He explained that reducing the time interval between the periodontal and endodontic treatment can be beneficial in these complex patient cases.
Latest Highlights from Instagram
Stay updated with our latest insights, highlights, and moments from the Academy.
Follow us on Instagram for event highlights, community stories, and inspiring clinical visuals.
EAED Website
Discover our mission, scientific program, and membership details on the official EAED site.
Stay up to date with news, events, and educational content from the EAED community.